- Closed as of Wednesday, 24th Dec 2025, re-opening Friday, 16th January 2026
- Request a Consultation for 2026
Choosing abdominoplasty is a careful, considered decision that extends well beyond the day of surgery. Recovery is where planning, teamwork, and small daily habits make a tangible difference. For people in Newcastle, Charlestown, and the wider Hunter region, Dr Yezdi Mistry approaches recovery as a structured process that respects individual variation while following sound clinical principles. The aim of this article is to provide a clear, practical roadmap for what most patients can expect after abdominoplasty, how to support healing sensibly, and when to seek help. It is educational in nature and does not replace personalised medical advice.
Dr Mistry is a Specialist Plastic and Reconstructive Surgeon with FRACS in Plastic Surgery. He established his private practice in Charlestown in 2017 after serving as a Visiting Medical Officer in hand and plastic surgery at John Hunter Hospital. His approach to postoperative care is patient focused, evidence informed, and measured. He prioritises preparation, clear instructions, and steady follow up so that recovery feels organised and predictable, even when individual timelines differ.
Abdominoplasty addresses redundant skin, laxity of the abdominal wall, or both. The recovery period involves more than wound healing. The body is adjusting to a new tissue arrangement. Muscles and fascia settle, swelling gradually resolves, and scars mature. Comfort improves in stages rather than in a straight line. Some days feel easier. Others feel slower. Setting expectations around this rhythm helps patients pace themselves.
The exact timeline depends on a number of factors. The extent of surgery, general health, nutrition, activity patterns, and whether additional procedures were performed all play roles. There is no single recovery clock that fits everyone. A good plan is individualised at the outset, reviewed at each appointment, and adjusted as needed.
Recovery begins in a monitored setting. The focus early on is comfort, gentle breathing exercises, and safe mobilisation with help. The abdomen feels tight and swollen. Dressings are checked regularly. If drains are used, they remove fluid from the space between the skin and the underlying tissue. The team explains how to position yourself in bed, how to support the abdomen when moving, and what to expect from the first walks.
Pain relief follows a multimodal plan. This typically includes paracetamol, anti inflammatory medication if appropriate, local anaesthetic use during the operation, and sometimes a nerve block such as a TAP block. The goal is to keep pain controlled enough that short, supported walks are possible. Early movement helps circulation and reduces the risk of complications such as clots. Hydration and light nutrition begin when you feel ready and when your surgeon gives the all clear.
Most patients leave hospital after one or two nights once pain is controlled and you can walk safely, eat light meals, and manage basic self care. Written instructions travel home with you so that nothing relies on memory.
The first week is about rest, routine, and gentle motion. Most people walk slightly flexed at the hips for several days because of tightness across the lower abdomen. This posture relaxes gradually as comfort improves. Short walks every hour or two while awake work better than long sessions. Think of movement as medicine delivered in frequent low doses.
A compression garment is typically worn. It provides external support and helps with comfort. Evidence for compression as a way to reduce fluid collections is mixed, but many patients report that they feel more supported when wearing it. The garment should fit snugly without causing increased pain or breathlessness. If it feels too tight, contact the clinic for guidance.
Incisions and drain sites need clean, dry care. The team will explain when you can shower, how to pat dry, and which dressings to use. Redness that spreads, increasing warmth, fever, or drainage with an odour warrants a call to the practice. Medication moves from stronger pain relief to milder options as the week passes. A simple bowel care plan reduces strain. Light meals with adequate protein and plenty of water support tissue repair.
Sleep works best with the upper body slightly elevated and a pillow under the knees. This position offsets abdominal tension. People who normally sleep on their side often add a pillow in front of the torso to reduce rotation. Small adjustments like these matter in the first days.
Energy improves and walking feels more natural. If drains are still in place, they are usually removed early in this window. Tenderness subsides although a sense of tightness remains because deeper layers are still healing. The garment remains part of the routine as recommended by the surgeon.
Most office based work becomes possible during this period, provided it does not involve heavy lifting or frequent twisting. Gentle household tasks return in stages. It is common to notice patches of altered sensation around the lower abdomen. These usually improve over time as nerves recover. The skin may feel puffy by evening and less so in the morning. That pattern reflects everyday variations in fluid movement and is expected.
Scar care often begins once wounds are closed and intact. Silicone gel or sheets can help limit thickening and colour change. Massage usually starts later, as advised by the team, once the skin tolerates gentle pressure. Sun protection is essential. Ultraviolet exposure can darken a healing scar. Clothing or high factor sunscreen avoids that risk.
Nutrition continues to be a quiet pillar of recovery. Aim for steady protein intake from fish, eggs, dairy, legumes, and lean meats. Include a colourful mix of vegetables and fruit for vitamin C and other micronutrients. Zinc plays a role in wound repair. Hydration aids comfort and reduces fatigue. Nicotine products significantly slow healing and are best avoided completely before and after surgery.
By this point, swelling has reduced but is not gone. The abdomen feels more mobile and the rate of day to day change is slower but steady. Many people resume office duties if they have not already done so. Light exercise returns gradually. Walking on an incline, a stationary bike with low resistance, and gentle stretching are typical starting points once the surgeon has cleared you.
Avoid heavy lifting and high core loads until you have explicit approval. The repair needs time to mature before it is asked to handle significant strain. Simple posture habits continue to help. Stand tall but do not force the posture. Use your hands or a folded towel across the abdomen when you cough or laugh to provide counter pressure.
Some patients ask about taping, lymphatic massage, or devices advertised for swelling or scar improvement. The research base is still developing. Taping protocols may provide comfort and assist with skin adherence for some people. Gentle lymphatic techniques can feel soothing and may help with fluid movement. These options should be discussed with your surgical team before you start. What suits one body at four weeks may not be suitable for another at the same time point.
Most daily activities are back in play by three months, with exercise volume increasing according to comfort and clearance. There is often a small but noticeable amount of residual swelling that softens month by month. Scar tissue continues to remodel. The colour lightens and the texture becomes flatter. Scar maturation can continue for a full year and sometimes longer. Patience matters here. The biology of healing has its own tempo.
Abdominal exercise is reintroduced cautiously. Early on this may mean breath led core activation, gentle pelvic tilts, and low load movements supervised by a physiotherapist when appropriate. The purpose is not to chase intensity. It is to restore coordination and endurance while respecting tissues that have been repaired. If an activity produces sharp pain or visible bulging along the incision, stop and seek advice.
Regular reviews with Dr Mistry’s team remain important throughout this phase. They allow ongoing assessment of scar behaviour, garment use, and activity progression. They also provide space to talk through daily challenges that do not always appear in handouts. Small adjustments to routine can improve comfort in a meaningful way.

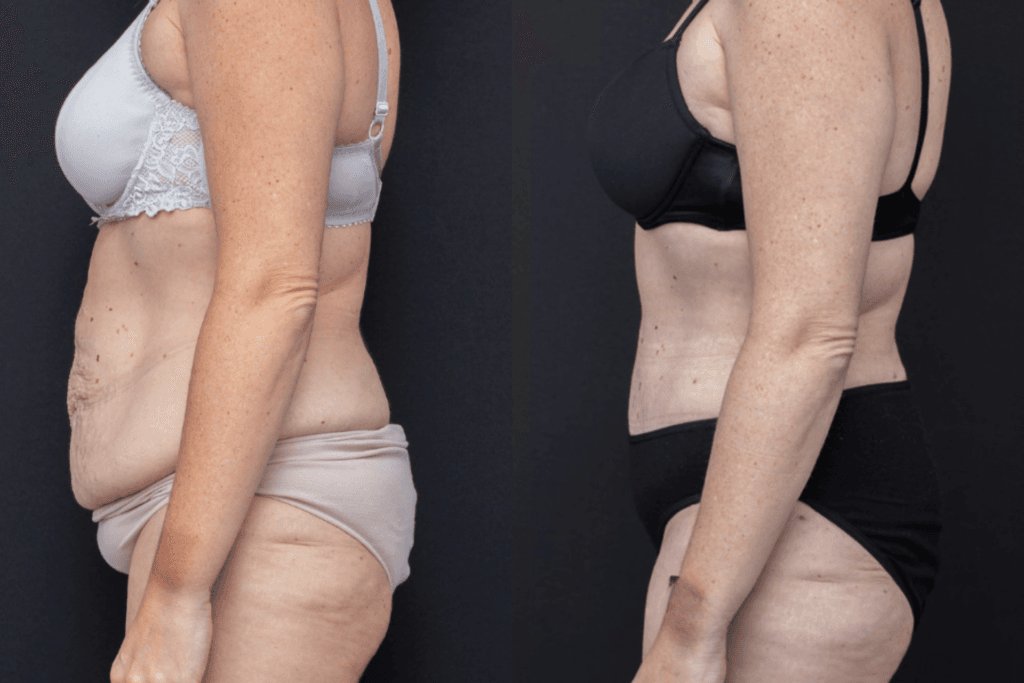
The outcomes shown are specific to those patients and may not reflect the results experienced by others, as individual outcomes can vary due to a range of factors.
Pain is expected after any operation on the abdominal wall. Most patients describe a strong ache that improves through the first week and then a pulling tightness that fades more slowly. A multimodal plan keeps discomfort manageable while limiting opioid use. This approach also helps with clear thinking, regular sleep, and early mobility.
Swelling follows a wave like pattern. It is commonly lower in the morning, higher late in the day, and increases with prolonged standing. Compression, gentle walking, and planned rests with the legs supported all help. It is normal to see small day to day shifts. The trend line is what matters. If swelling increases suddenly, becomes asymmetric, or is accompanied by redness and heat, call the practice.
Altered sensation is common. Nerves that carry touch and temperature signals were disturbed during surgery. They regenerate slowly. Tingling, patchy numbness, or hypersensitive areas often appear during this process. Most changes improve over several months. Small regions of reduced sensation may persist. This is usually not limiting in daily life, but it is useful to know so you can take care with heat exposure and hair removal near the incision.
Scars are an expected and permanent record of any surgery. The aim is to guide that record toward a flat, soft, pale line over time. Placement is low across the abdomen so it generally sits beneath underwear or swimwear. Early appearance is pink and slightly raised. Later it cools in colour and flattens.
Silicone products are well supported by evidence for reducing thickness and colour intensity when used consistently on closed, intact skin. They are easy to incorporate into a routine. Massage comes later and is introduced gently. Firm pressure too early can irritate tissue. Sun protection makes a large difference. A hat and clothing are best. A broad spectrum, high SPF sunscreen is useful for any incidental exposure.
If a segment of scar becomes raised or firm beyond what is expected, there are options to help such as extended silicone use, pressure techniques, or specific treatments in clinic. Early identification leads to better outcomes. Bring any concerns to your review appointment rather than waiting to see if they settle on their own.
Nutrition, sleep, and daily rhythm are not side notes. They are central to recovery. Aim for regular meals that combine protein, complex carbohydrates, and healthy fats. Include a variety of vegetables and fruit. Keep a water bottle within easy reach. Limit alcohol while you are on prescription medication and in the early postoperative period more generally.
Plan your day in small blocks. Alternate activity with rest. A twenty minute walk followed by time with your feet up works better than a single long push. Keep items you use frequently at waist height to avoid bending or reaching. Accept help when it is offered, particularly for shopping and chores in the first weeks.
Smoking and nicotine products restrict blood flow. They are strongly associated with slower wound healing and a higher rate of wound problems. If you need support to stop, ask the team for resources well before your surgery date.
Office based work usually resumes between two and four weeks, with adjustments for fatigue and posture. Roles that involve lifting, prolonged standing, or sudden movements require a longer pause. Your surgeon will guide timing for your specific situation. It is safer to stage the return than to press for an early date that risks setback.
Exercise follows a similar principle. Start with walking. Add low resistance cycling. Introduce gentle mobility work. Strength training returns later with practitioner approval. Think about three levers you can adjust at each step. These are intensity, volume, and frequency. Increase only one at a time. If you are comfortable at a given level for a full week with no adverse signs, then move the next lever by a small amount.
Most recoveries progress without serious issues. Knowing when to ask for help ensures that potential problems are addressed early. Contact Dr Mistry’s team if you have increasing redness or warmth around the incision, a fever, a sudden surge in swelling, shortness of breath, calf pain, or pain that does not respond to the plan you were given. Trust your instincts. If something feels wrong, it is better to call and be reassured than to wait.
Many people feel ready for office work by two to four weeks, light exercise by four to eight weeks, and broader activity by three months. Some move faster, others slower. Larger procedures and combined operations usually extend the timeline. It is normal for appearance to keep evolving for six months or longer as swelling recedes and tissues soften. Setting realistic expectations at the start prevents unnecessary worry and supports sensible pacing.
Preparation starts well before the operation. At your preoperative visit, measurements are taken, risks are explained clearly, and you receive a written plan. You leave with information about garments, medication, movement, and follow up dates. On the day of surgery, the operative plan is reviewed once more. After surgery, you are seen on the ward and again at regular intervals once you are home. The practice is located in Charlestown, within easy reach of central Newcastle and the surrounding suburbs, so returning for review is straightforward.
Communication is a priority. The clinic provides contact details and clear instructions for after hours concerns. If you are unsure about a symptom, a garment fit, or an activity choice, you can ask. Small queries answered early keep recovery on track.
Questions often arise about lymphatic massage, taping, laser therapies, and supplements. The evidence for some of these is evolving. Gentle lymphatic techniques delivered by a trained practitioner can be considered once the surgeon confirms that the timing is appropriate. Taping may provide comfort and support for skin adherence in selected cases. Low level light therapies are studied in other surgical areas and may have a role, but they are not standard care after abdominoplasty. Supplements should not be started without discussion because some products affect bleeding, swelling, or medication interactions. A cautious approach that prioritises established measures is sensible.
Tightness is most noticeable in the first few weeks and gradually eases as the deep layers of the abdominal wall heal. Most patients feel a natural softening by three months, though mild firmness can persist for several more months.
Yes. Temporary numbness or tingling near the incision is common because small nerves are stretched or divided during surgery. Sensation usually improves within several months as the nerves regenerate.
Driving can generally resume once you can wear a seatbelt comfortably, move freely, and react quickly without pain. This often occurs after two to three weeks, but the timing varies between individuals.
Short, gentle walks promote circulation and help reduce the risk of complications such as blood clots. Early movement also assists in maintaining lung expansion and supports a smoother return to normal mobility.
The garment is usually worn for several weeks, depending on your surgeon’s advice. It provides support and comfort as swelling decreases and tissues settle into their new position.
Yes. Swelling often fluctuates throughout the day, especially with extended standing or activity. Elevating your legs and maintaining hydration can help manage this normal variation.
They should be avoided until your surgeon confirms the abdominal wall has healed adequately. Light core engagement may begin gradually under supervision once cleared, often after several weeks or months.
Smoking, poor nutrition, infection, or returning to heavy activity too soon can all slow recovery. Following post-operative instructions carefully helps minimise these risks.
No. Scar appearance depends on genetics, skin type, surgical technique, and ongoing care. Consistent use of silicone gel or sheeting and sun protection can help scars mature more evenly.
Increasing redness, heat, or swelling around the incision, fever, shortness of breath, or pain not relieved by medication should prompt immediate contact with your surgical team. Early assessment prevents small issues from becoming larger concerns.
Recovery continues after the first few months. Tissues keep maturing and the abdomen settles as swelling fades. Ongoing follow up allows small adjustments that improve comfort, garment use, and activity planning. Patients in Newcastle and the Hunter region who would like further information about recovery after abdominoplasty or other plastic and reconstructive procedures are welcome to contact the practice in Charlestown.
Dr Yezdi Mistry | Specialist Plastic & Reconstructive Surgeon
AHPRA Registration: MED0001861566
Charlestown Consulting Rooms
Suite 312, Level 3
99 Pacific Highway
Charlestown NSW 2290
Phone: 02 4062 7888
Email: admin@drmistry.com.au
Website: www.drmistry.com.au
All surgical and invasive procedures carry risks such as bleeding, infection, fluid collections, delayed wound healing, and venous thrombosis. Risk is influenced by personal health factors and by the scale of the operation. The purpose of preoperative assessment is to identify and reduce modifiable risks wherever possible. The information provided here is general and cannot account for every situation. Decisions about surgery and recovery pathways should be made in consultation with a qualified specialist plastic surgeon who has assessed you in person.
Recovery after abdominoplasty is NOT a race. It is a series of small, well chosen steps that build on each other. Good preparation, clear instructions, and consistent follow up make those steps easier to take. Dr Yezdi Mistry and his team in Charlestown provide a structured pathway that respects individual variation and aligns with current clinical evidence. With sensible pacing, attention to nutrition and movement, and timely communication with your surgical team, most people navigate recovery steadily and return to their usual routines with confidence in their day to day comfort.

Dr Yezdi Mistry is a Specialist Plastic and Reconstructive Surgeon based in Newcastle, NSW. With extensive training and experience in both reconstructive and aesthetic surgery, Dr Mistry is committed to providing safe, evidence-based care that is tailored to each patient’s individual needs.
After completing his Fellowship of the Royal Australasian College of Surgeons (FRACS) in Plastic Surgery in 2013, Dr Mistry relocated to Newcastle with his family in 2015. He began his work as a Visiting Medical Officer (VMO) in Plastic and Hand Surgery at John Hunter Hospital before establishing his private practice in 2017. His practice offers a comprehensive range of reconstructive and aesthetic procedures for the breast, body, face, and skin.
Dr Mistry’s approach to patient care is grounded in trust, respect, and open communication. From initial consultation to recovery, he aims to ensure patients feel informed, supported, and comfortable throughout their surgical journey. He is dedicated to maintaining the highest professional and ethical standards in all aspects of his work.
To remain at the forefront of modern surgical techniques, Dr Mistry continues to pursue ongoing professional development both in Australia and internationally. He was Australia’s first delegate at the Body Contouring Academy in Paris, where he received advanced training in body contouring and skin-tightening techniques, including VASER and RENUVION technologies.
Fill in your details and our friendly team will be in touch with you
Please Note: Information provided on Dr Mistry’s website is provided as a basic guide, it does not constitute a diagnosis and should not be taken as medical advice. Any surgical or invasive procedure carries risks.




“I care because it’s my job as a surgeon, as a plastic surgeon, to do the appropriate thing and to give you a good outcome. I want to leave knowing that I can tell a patient, hand on heart, that I did the very best I could and that I looked after them, so when I see them post op later that day or the next morning, that they feel they were in good hands.”
– Dr Yezdi Mistry
Request a Consult