- Closed as of Wednesday, 24th Dec 2025, re-opening Friday, 16th January 2026
- Request a Consultation for 2026
Recovering from an arm lift, or brachioplasty, is a gradual and structured process that allows patients to safely return to normal activities while the body heals. The recovery period combines surgical healing, tissue adaptation, and careful post-operative care. Understanding what to expect after surgery helps patients prepare both physically and mentally.
This article draws on current medical literature and the clinical experience of Dr Yezdi Mistry, Specialist Plastic and Reconstructive Surgeon, to outline the stages of recovery after arm lift surgery. It highlights how the body heals, how to care for the incisions, and what patients can realistically expect over time.
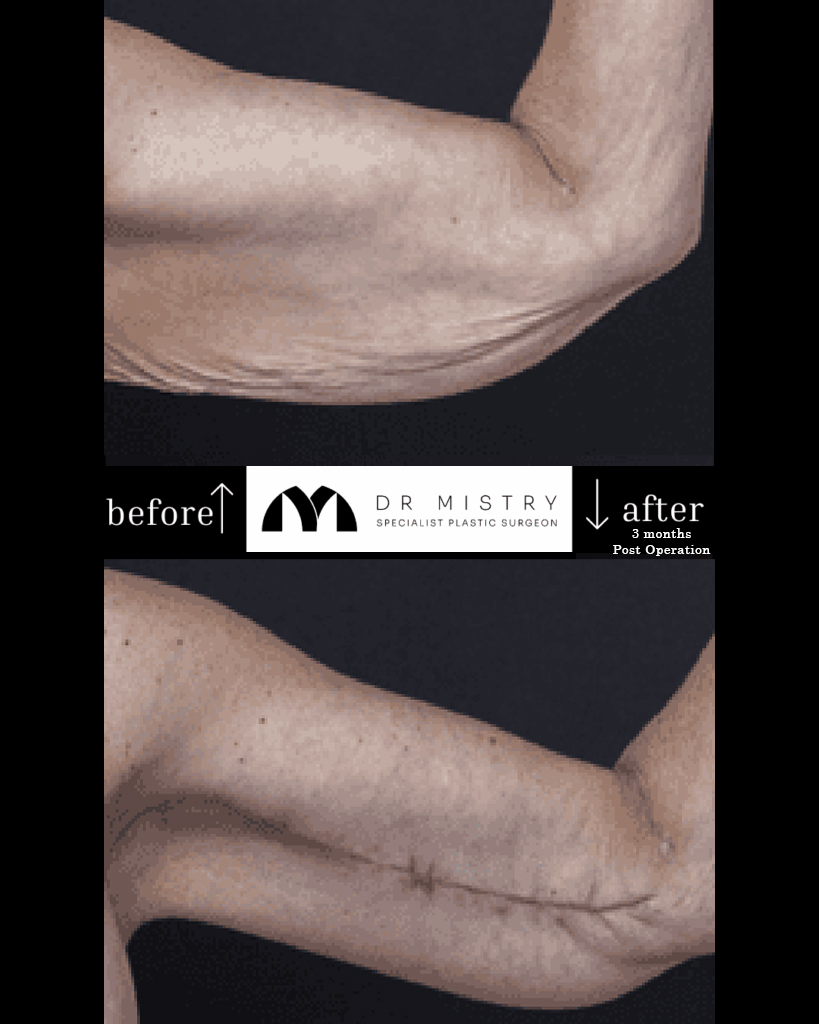
An arm lift removes excess skin and soft tissue from the upper arm, typically extending from the underarm to the elbow. The aim is to reshape the area by tightening and redraping the remaining skin. This procedure is often sought by people who have lost significant weight or whose skin elasticity has reduced due to ageing.
The method of recovery depends on several factors, including the surgical technique, the extent of tissue removal, the patient’s health, and whether liposuction was performed. Research published in Aesthetic Plastic Surgery (2025) compared incision placements and found that the postero-medial approach balanced scar concealment with patient comfort during recovery.
Every patient heals at a unique pace. Dr Yezdi Mistry, Specialist Plastic and Reconstructive Surgeon, emphasises that recovery is influenced by factors such as general health, skin condition, and adherence to post-operative instructions. For most patients, light daily activities resume within two weeks, while more vigorous movement takes several weeks longer.
The first few days after surgery are critical for rest and wound protection. The arms are wrapped in light dressings or compression sleeves, and some patients may have small drains to remove fluid. Swelling, bruising, and discomfort are common during this time.
Keeping the arms slightly elevated on pillows helps reduce swelling. Patients are encouraged to rest but also to take short walks to improve circulation and reduce the risk of blood clots. Pain medication is prescribed as needed, and hydration and balanced nutrition support healing.
Follow-up appointments during this period allow the surgical team to check incisions, remove drains, and ensure early healing is progressing well. Clean, dry dressings and gentle movement of the arms help prevent stiffness while protecting the surgical sites.
Within the first two weeks, most patients notice a reduction in bruising and swelling. Compression garments remain important during this time because they help limit swelling and support the tissues as they settle. The incisions are still delicate, and the arms may feel tight as the skin adjusts.
Light movements are reintroduced gradually to maintain flexibility, but heavy lifting and reaching overhead should be avoided. A balanced diet with sufficient protein, vitamins, and minerals aids wound repair. Smoking and alcohol should be avoided, as both slow healing and increase the risk of infection.
Dr Yezdi Mistry, Specialist Plastic and Reconstructive Surgeon, advises patients to watch for redness, fluid accumulation, or warmth around the incision lines. Early signs of infection or seroma should be reported promptly so they can be treated before complications arise.
By the third week, patients usually experience improved mobility and comfort. The majority of swelling subsides, and normal daily activities can gradually resume. The compression garment continues to provide gentle support, although it may only be needed part of the day.
Scar healing progresses, and silicone gels or sheets may be introduced once the wounds have closed fully. Incisions can appear pink or raised during this period but typically soften as healing continues. Patients with desk-based work often return to their roles after two to three weeks, while those with more physical occupations may need four to six weeks before resuming.
Driving is usually permitted once the patient can comfortably move their arms without pain or stiffness. It is important to continue protecting the incisions from friction and to avoid exercise that strains the arms until advised by the surgeon.
From the third month onward, scar maturation becomes the focus. Scars gradually fade and flatten, though complete softening can take up to a year. Some temporary numbness or firmness may persist but usually improves as nerve endings regenerate.
Sun protection is crucial. Scars exposed to sunlight too early may darken permanently, so sunscreen or protective clothing is recommended. Patients may also continue wearing compression garments at night for a few months if swelling persists.
Dr Yezdi Mistry, Specialist Plastic and Reconstructive Surgeon, notes that maintaining a stable weight is one of the most effective ways to preserve results. Large fluctuations in weight can stretch the skin again. Regular physical activity, good nutrition, and consistent hydration all support tissue health and overall comfort.
Psychological recovery is also part of this phase. As arm strength returns and swelling subsides, patients begin to appreciate the improved contour and feel more at ease performing everyday activities.

While most recoveries progress smoothly, it is important to recognise symptoms that require medical attention. Persistent pain, redness, drainage, or sudden swelling should prompt review. In medical studies of over 1,000 arm lift patients, around one-quarter experienced minor wound complications such as delayed healing or fluid accumulation, which were typically managed without further surgery.
Regular follow-up appointments are essential. Dr Yezdi Mistry, Specialist Plastic and Reconstructive Surgeon, advises attending each review, even if recovery appears normal. These visits allow the surgeon to assess scar progress, monitor swelling, and ensure the arms are healing as expected. Early intervention is key to preventing small issues from becoming larger concerns.
Successful recovery relies on more than rest. Nutrition, hydration, and gentle movement all contribute to healing. A diet rich in lean protein, fruit, vegetables, and healthy fats supports collagen production and tissue repair. Adequate water intake keeps the skin supple and reduces inflammation.
Resting with the arms elevated helps swelling subside, while slow, controlled arm movements prevent stiffness. Patients are encouraged to avoid wearing tight or restrictive clothing over the incision lines, as friction can irritate healing skin.
Sleep position also plays a role. Resting on the back with arms supported by pillows minimises strain on the incisions. Patients should avoid sleeping on their sides for several weeks to prevent pressure on the healing tissues.
Lifestyle choices greatly affect both the pace and quality of healing. Smoking and nicotine products reduce oxygen flow to the tissues and delay wound repair. Quitting before and after surgery is strongly recommended to minimise complications. Alcohol can also interfere with medications and increase inflammation, so limiting intake is beneficial.
Nutrients such as vitamins A and C, zinc, and iron are especially important in recovery. Incorporating foods like fish, leafy greens, citrus fruit, and whole grains supports immune function and cell renewal.
Emotional wellbeing is another key factor. It is natural for patients to feel temporary frustration during recovery when healing feels slow. Setting realistic expectations and maintaining open communication with the surgical team help maintain perspective and reassurance.
Light activity, such as walking, can begin soon after surgery. More demanding exercise, including lifting weights or performing overhead motions, should wait until the surgeon confirms that healing is sufficient.
Gentle stretching and physiotherapy can start two to three weeks post-surgery, depending on the individual’s progress. Activities that involve impact or strong upper-body engagement are generally postponed for at least six weeks. Pushing activity too early can disrupt incisions or widen scars.
Each patient’s recovery plan is customised. Some may return to exercise sooner, while others require additional time. Listening to the body and following medical advice are the safest ways to restore movement and strength without affecting results.
Once the initial healing is complete, long-term care focuses on preserving results. Regular check-ups help ensure that scars are settling properly and that no late issues arise. Follow-up visits usually occur at one week, one month, three months, six months, and one year after surgery.
Scar care may include silicone treatments, massage, or other topical products as directed. These measures encourage softening and even colouring of the scar tissue over time. Continued protection from the sun is also advised for at least twelve months.
Maintaining a steady weight, eating well, and exercising regularly all help sustain the surgical outcome. Patients often find that committing to healthy routines supports their overall wellbeing long after the initial recovery phase.
Most patients can begin gentle arm elevation after two to three weeks, once initial healing is stable. Full overhead movement typically returns after six weeks, depending on individual progress and surgeon advice.
The scars are permanent but usually fade and flatten over time. Their visibility depends on factors such as incision placement, genetics, and adherence to scar care instructions.
It is best to avoid side-sleeping for the first few weeks to reduce pressure on the arms. Sleeping on your back with arms supported by pillows helps minimise swelling and tension on the incisions.
Yes, temporary numbness or tingling can occur due to nerve irritation during surgery. Sensation usually improves over several months as nerves recover.
Swimming should be avoided until the incisions are fully healed and closed, which usually takes six to eight weeks. Always confirm with your surgeon before resuming water activities.
Residual swelling is common and often linked to individual healing patterns, activity levels, or lymphatic function. Wearing compression garments and following movement guidelines helps reduce lingering swelling.
Yes, overexertion can strain healing tissues and widen scars. It is safest to wait until cleared by your surgeon before resuming intense workouts.
Most patients benefit from wearing them for at least four to six weeks, sometimes longer if swelling persists. The duration is tailored to each person’s recovery and comfort.
Persistent redness, warmth, fluid drainage, fever, or sudden swelling around the incision should be reviewed promptly. These can signal infection or fluid collection requiring medical attention.
Although early improvements appear within weeks, final results become clearer around nine to twelve months. This allows time for scars to mature and tissues to fully settle.
Healing after arm lift surgery is a process that unfolds gradually over several months. While noticeable improvements occur within the first few weeks, complete recovery and final results develop over time. Patients who follow their post-operative plan closely and maintain healthy habits generally experience smoother healing and greater comfort.
Recovery is unique to each person, influenced by their age, health, and commitment to aftercare. Consistent communication with the surgical team helps manage expectations and ensures that healing progresses appropriately.
For those seeking further information or wishing to discuss individual recovery needs, Dr Yezdi Mistry, Specialist Plastic and Reconstructive Surgeon, welcomes consultations at his Charlestown clinic. His practice serves patients throughout Newcastle and the Hunter region.
To learn more or book an appointment, contact:
Dr Yezdi Mistry, Specialist Plastic and Reconstructive Surgeon
Charlestown Consulting Rooms
Suite 312, Level 3
99 Pacific Highway
Charlestown NSW 2290
Phone: 02 4062 7888
Email: admin@drmistry.com.au
Website: www.drmistry.com.au
Through evidence-based care and patient-focused guidance, Dr Mistry and his team support each stage of recovery with professionalism and attention to detail. Patients can expect a structured healing experience built on safety, understanding, and clinical best practice.

Dr Yezdi Mistry is a Specialist Plastic and Reconstructive Surgeon based in Newcastle, NSW. With extensive training and experience in both reconstructive and aesthetic surgery, Dr Mistry is committed to providing safe, evidence-based care that is tailored to each patient’s individual needs.
After completing his Fellowship of the Royal Australasian College of Surgeons (FRACS) in Plastic Surgery in 2013, Dr Mistry relocated to Newcastle with his family in 2015. He began his work as a Visiting Medical Officer (VMO) in Plastic and Hand Surgery at John Hunter Hospital before establishing his private practice in 2017. His practice offers a comprehensive range of reconstructive and aesthetic procedures for the breast, body, face, and skin.
Dr Mistry’s approach to patient care is grounded in trust, respect, and open communication. From initial consultation to recovery, he aims to ensure patients feel informed, supported, and comfortable throughout their surgical journey. He is dedicated to maintaining the highest professional and ethical standards in all aspects of his work.
To remain at the forefront of modern surgical techniques, Dr Mistry continues to pursue ongoing professional development both in Australia and internationally. He was Australia’s first delegate at the Body Contouring Academy in Paris, where he received advanced training in body contouring and skin-tightening techniques, including VASER and RENUVION technologies.
Fill in your details and our friendly team will be in touch with you
Please Note: Information provided on Dr Mistry’s website is provided as a basic guide, it does not constitute a diagnosis and should not be taken as medical advice. Any surgical or invasive procedure carries risks.




“I care because it’s my job as a surgeon, as a plastic surgeon, to do the appropriate thing and to give you a good outcome. I want to leave knowing that I can tell a patient, hand on heart, that I did the very best I could and that I looked after them, so when I see them post op later that day or the next morning, that they feel they were in good hands.”
– Dr Yezdi Mistry
Request a Consult